A couple weeks ago, we asked how COVID-19 was affecting your practice . . .
. . . and I thought you might like to know what we found out.
But first, thank you to the hundreds of practitioners from across the globe who shared their experiences. This helps us better understand how we can support you during the pandemic.
Now, let’s get to it. What did we learn? Well, first, we asked:
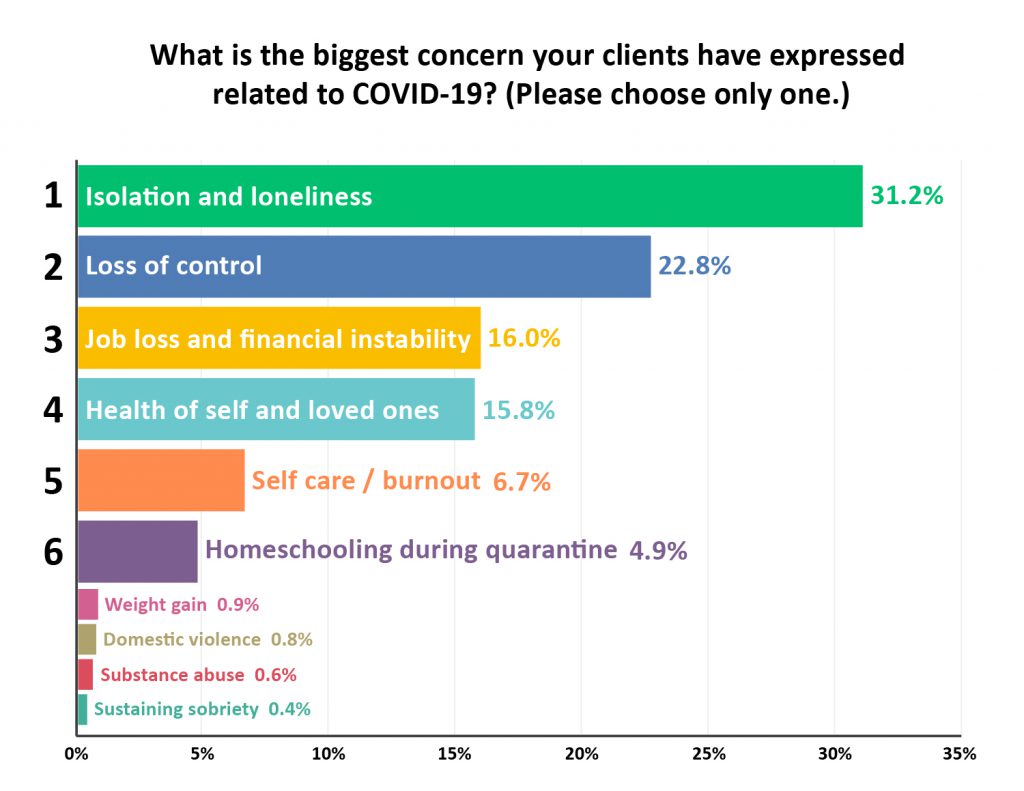
Isolation and loneliness (31%) followed by Loss of control (23%) are top concerns right now for patients.
The pandemic poses many new relational challenges – especially for clients who already struggled to connect with others.
If your clients are feeling lonely as they practice social-distancing, here are some creative strategies for fending off loneliness and keeping relationships strong. Next, we asked:
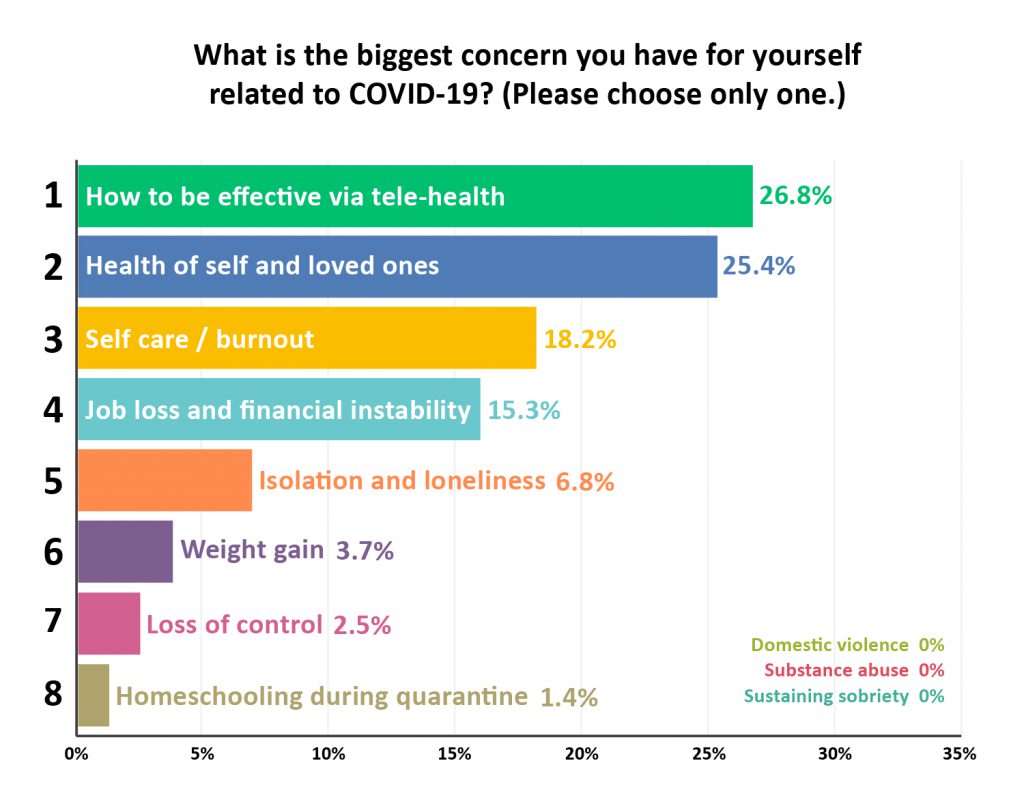
For practitioners, some of the biggest concerns were How to be effective via tele-health (27%) and the Health of self and loved ones (25%).
Even experienced practitioners can find online sessions challenging. It can be harder to connect with a client, and sometimes your most effective interventions don’t translate easily to online work.
Beyond that, online sessions can be surprisingly exhausting.
For some practical ways to beat Zoom fatigue and make the transition to tele-health easier for you and your clients, check out our recent blog, Practical Ways to Improve Telehealth Sessions.
Next, we looked at clinical issues:
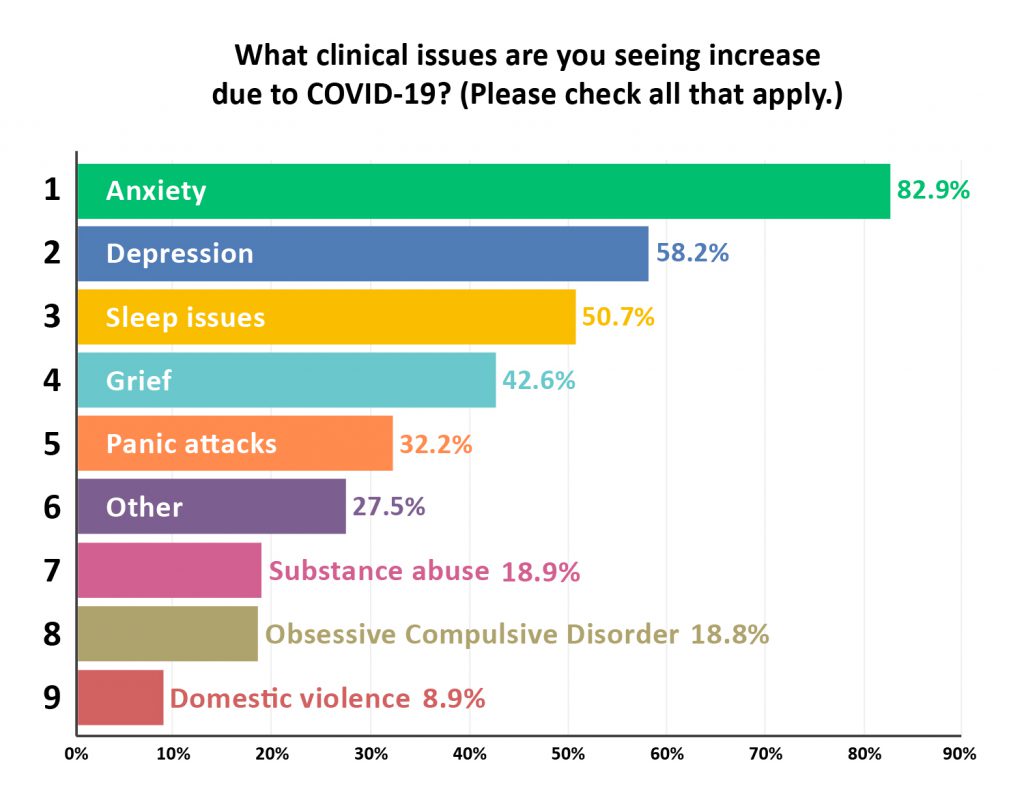
The pandemic brings a whole new set of challenges to clinical work. We have to adapt interventions to be effective during social-distancing and quarantine.
As we all face a lot of uncertainty about the future, it’s no surprise that Anxiety (83%) is increasing significantly among patients.
If you’re looking for strategies to help patients get relief from anxiety right now, you may want to check out this conversation I had with Christine Padesky, PhD, and Ron Siegel, PsyD. Click here to hear their strategies for alleviating worry during COVID-19.
The majority of practitioners are also seeing Depression (58%) and Sleep Issues (51%) increase.
Joan Borysenko, PhD and Rick Hanson, PhD recently shared some thoughts on the sense of sadness and loss that’s become so pervasive during the COVID-19 pandemic. You can hear the full story here.
We believe that the work being done by mental health practitioners is especially critical as we go through the pandemic.
That’s why we’ve made it our mission to support you with ideas from some of the world’s top experts.
Keep an eye out for more strategies for clinical practice during COVID-19 coming out soon.
Now we’d like to hear from you. If there’s any question you have for the experts, or any topic that you’d like to see on an upcoming blog, please let us know in the comments.
Hi,
while I’m seeing Anxiety increase at this stage of Covid-19, it is the type that is challenging. Many of my clients had Social Anxiety going into the pandemic and found relief when social distancing/isolation came into play. As restrictions are lifting, Anxiety has become Agoraphobia, and work we were progressing on before now has to shift to exposure therapy. Exposure therapy with a somatic/vagal awareness and support approach would be helpful.
Thank you for all you do,
Teresa (BC, Canada)
I would love to see a blog about when and how other therapists plan to go back to face to face sessions.
Agreed!!! I have tried to research this on my own and get conflicting answers. APA and The Trust liability insurance have useful information and consent forms. I feel masks are important now but not conducive to the work of therapy. I am concerned about asymptomatic transmission from clients and from myself to clients. I would feel safer with continuation of teletherapy and find it just as effective if not more, as long as clients can get privacy at home. However, I feel internal pressure to return to the office. I also miss that therapeutic space because I think it helped with burn out.
I’d love to see the survey divided into those that do and don’t have young kids with corresponding stress levels; its two totally different worlds.
I would love to see best practices for doing trauma work via telemental health. Also how are practitioners handling family sessions?
Thank you for always keeping us informed. Great information!!
Anxiety and depression are by far the most common complaints our clients have. What is surprising to me is that domestic violence is so low on the list, whereas I hear from my clients a lot of stories about this topic. Maybe people are ashamed to admit it; maybe some or most of the violence is psychological and verbal and not physical and so it is not reported.
Thank you for the information breakdown, resources and data reflections Ruth. Always useful and enlightening to see changes / behaviors in clients (and practitioners) in times of crisis. Allows some preparation for myself and clients towards future events as well as the situation facing the world at present.
Wow, THANK YOU so much! Concise, relevant, most helpful! Not surprising but good to see it confirmed. Something concrete I can take away and show others in my field, which is non-clinical support. Much gratitude …
I have a dramatic story I’d like to share. I already mentioned that due to the rural area where i live and the age of so many of my clients, most were already in the home alone or with family members, only occasionally going out for shopping and medical appointments. Their adjustments have been less jolting. But I did mention that having kids at home was a strain for some mothers and that kids are not happy.
Well, one mother wasn’t having a problem with homeschooling her son because she had done it when he was younger. This boy, now 16, was a client of mine for about 3 years in his tweens. He was suffering from PTSD, depressed, angry, disobedient, non-cooperative with his mother, rebelling toward his homeschooling and rejecting of his step-father who he refused to consider as a father.
Through treatment for abuse by his biological father and considerable joint therapy with his mother, his behavior improved greatly. He has been able to go to a Christian school for junior high where he made many friends and has consistently gotten straight A’s, something he has been proud of. He also has developed a close bond with his step-father with whom he goes to a weekly father and sons Christian group. Over these years, he has been coming home from school feeling happy, cooperative, helpful and pleasant (most of the time – he is still a teen.)
Now comes COVID-19.
His school closed, of course, and he was back to home schooling and could see none of his many friends. Within days his behavior regressed to what we had see when he was a tween. His mother, who is still my client, was back to feeling at whits ends and as if she has lost her son again. The situation was growing worse day to day.
Last week his Christian school offered to allow children who desired to return to their school rooms, (against the state orders but with all the required safety measures). With some trepidation, his parents agreed with his desire to return. Although there are only 4 other children in the class room who have to follow social distancing and wear masks, suddenly he is the person he’s been for the past few years. His mother reports he’s coming home happy everyday and is being a cooperative, enjoyable member of the family.
Of course the school should not be defying the state order but, my goodness, what a blessing this has been for this boy and his family. We all hope they will stay physically healthy as well.
I shared this story because it is such a clear example of the negative effect social isolation is having on our youth and with a hope that schools will develop innovative ways to make in-school attendance safe again, i.e. staggered in-school days or different configurations of school hours along with part-time distance learning.
This is what keeps me up at night. Witnessing the developmental interruption of younger children who have less of a point of reference for their contact. Thank goodness the family you refer to had the sense to do what was needed. The combination of stressed parents and stressed kids is a painful stew!! If strung out too long, the potential for damaging attachment is real.
Thank you
Thank you!
I am deeply moved as I witness your continuing, persistent efforts to inform and support this community of practitioners. You never give up in reaching out, in this altruistic expression of caring toward people “in the field” – those who are on the front lines of helping others in need.
Thank you to the speakers for all of their insight. It was nice to be able to put some new definitions around many of what we and our clients are going through at this time that is relatable.
Wow the feedback from those questions is really helpful. Thank you!
This was very reassuring! Being isolated from my colleagues, outside of a brief staff meeting a couple times a week, one can feel that what they’re experiencing is unique to them. It is sad in so many respects though also very helpful to know that I am not alone in what I’m feeling.
Thank you!
Excellent! This was helpful information and I love that you provided resources for some of the main issues that have been arising among practitioners and clients.
Personally, I only do phone sessions during Covid. I do not do video as I find it has some major drawbacks:
People are more self-conscious, whether they’re aware of that or not, and more likely to disclose less.
I personally find it exhausting to stare into a screen all day.
Unlike sitting with someone in my office, the unrelenting forced facial focus also enervated the other person.
I have been doing phone sessions for decades with people who don’t live locally or who moved out of town, and they are even more effective, sometimes, than ones held in my office. I think the reason for this is I am actually not looking at them and they feel far freer, just as in Freud’s day, unloading and sharing things they might not otherwise feel comfortable talking about.
One of my colleagues suggested that using a video link mirrors the misalignment to the mother that insecure patients experienced during infancy – ie the delay (although it is very minor these days) and also the fact that eye contact is not really possible because we look a the face and not the camera. It was an interesting comment. I find some clients are very happy using video conferencing but some, as you say Nicole, feel stressed by it. I thought I would offer the thoughts! I’m not a fan myself but I do use it when I need to.
I use the zoom background feature
– a photo of a corner of my Workplace office. So when using the video feature, It looks like I’m in the garden corner. Patients comment that it is familiar and comforting to them. Attendance is up, as many finds the telehealth convenient. I like seeing where they set up for privacy.
I also found that phone conversations are very satisfying for many clients. But for me they are problematic as I want to see gestures, body language, facial expressions etc. As an alternative when we cannot have real physical meetings they are better than nothing, but I cannot really say that they satisfy me.
Thank you very much for this information.
My patients definitely have anxiety but it’s interesting that some have anxiety related to returning to work.
They see the stay at home mandate as perfect for them.
I’m in Massachusetts
Any information on parenting and anxiety might be helpful.
Thank you for the great information and insights.
Thank you!
I’ve only glanced at all this – but wouldn’t it be nice to include the good sides too? I think there are advantages both to myself and clients in lock down. Stillness – time to reflect – getting off the rat wheel – consuming less – enjoying better air – beautiful spring weather – good home cooking – more time with loved ones – to name but a few.
I tire of the constant pathologising. Our world cannot go on this way – our ecosystems are dying and climate change threatens us all. This is a wake up call. Time to reflect.
My work focuses on families and children-I would appreciate a program that focuses on effectively using zoom with this population. Thank you.
Thanks for this support. I do have questions about how poly vagal interventions with clients with PTSD, particularly physical presence and proximity, might work in this format?
Thanks again,
I’d like to see some discussion about what are the practical, emotional factors we need to consider if and when we start to even think about face to face sessions. My lovely counselling room is windowless and small leading me to wonder if I’ll ever feel comfortable using it again and maybe having to relocate. Also, part of my work involves working with children in school; what measures are we thinking about to help provide a safe therapeutic environment – removing all the soft, tactile resources, wearing masks ?…is there room for perspective??
Thank you once again for the resources you so carefully and skilfully offer. As Covid-19 is now ramping up in SA, I anticipate seeing more fear, stress, anxiety and depression. For now, my experience as a clinician, working with a middle to upper middle class population, has mostly been that of client’s old wounds reemerging in the isolation and an intense engagement with them. In this sense lockdown has provided helpful healing possibilities, if somewhat destabilising. However, I am feeling a “girding” of myself for the likely onslaught of what is still to come in our country and the collegial spirit I feel when listening to the interviews is helpful. Thank you
This is great. Thank you!
Thank you for continuing to be a resource. It’s particularly useful that you checked in with practitioners for information and feedback and then are directing resources accordingly.
Many of us are at the front lines of the behavioral health issues of this pandemic.
Mental health offers integrative medicine which can make all the difference.
I’ve discovered so many unique benefits and opportunities during this time. Life changing insights and transformations for my patients as well.
The telemedicine has afforded unique opportunities that I could not have envisioned. Seeing patients in their homes, cars, or wherever they are, hasn’t been a distraction at all. It’s been a tremendous opportunity actually. So much so that I’m going to use it as part of my practice even once the pandemic settles.
Thank you.